Medicare’s 2026 Physician Fee Schedule (PFS) will improve how you deliver and are compensated for implementing and managing Remote Patient Monitoring (RPM). These changes are in response to feedback provided on the current program. The two new codes fill the gap when patients don’t meet the current threshold of 16 readings and 20 minutes.
Here’s why it matters and what to do next.
Under the current RPM program, if a patient uses the provided device for less than 16 days in a month, you cannot bill for that particular code. Similarly, if you spend less than 20 minutes with a patient in a month, billing is not permitted under that code. As a result, you may be delivering significant value without receiving compensation.
Meet the New Device & Management Codes
CPT Code 99445
- New 2 to 15-day device-supply code (CPT code 99445) Average Medicare reimbursement of $47*. This new code compensates you for supplying devices to patients who transmit data for just a couple of days each month. This change recognizes that there is still value for patients even if they are not hitting 16 days each month.
- 99454 is the current code, now reserved for patients with 16–30 days of device use per 30-day increment. Average Medicare reimbursement of $47*. Using both codes will allow compensation for a larger number of patients in the program.
CPT Code 99470
- New 10-minute RPM management code (CPT code 99470) Average Medicare reimbursement of $26*. This code covers 10-minutes of clinical staff time that includes at least one interactive communication. This acknowledges that meaningful, impactful touchpoints don’t always stretch to 20 minutes. This patch fills the gap.
- 99457 (initial) and 99458 (add-on) are the current codes used for 20-minutes of clinical staff time and remain in place—so you can bill for whichever option reflects real care time.
With the addition of these new codes, you will be able to bill for more of the patients you have in the program – getting reimbursed for more of the care you deliver.
Implementing the New RPM Guidelines
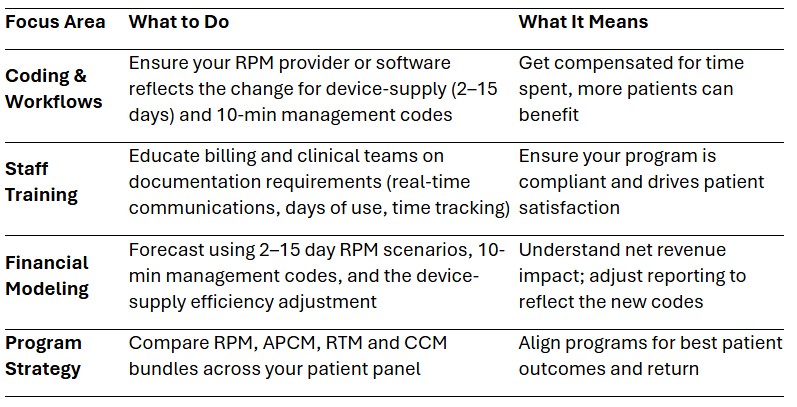
What This Means at the Patient Level
- Expanded access: Even patients who do not, or cannot, commit to 16+ days can still be enrolled and benefit from the program
- Less time commitment: A brief check-in, rather than 20 minutes, can now be captured and billed, promoting early intervention and adherence.
The 2026 PFS Final rule further unlocks the clinical value of RPM for patients and eliminates some of the barriers for providers looking to improve outcomes for those in their care.
Have questions?
We’re here to help! Reach out to RemetricHealth to implement the new changes, get support for your current program, or learn about new programs like APCM. RemetricHealth makes care management programs easier for your practice and your patients.
* Average nominal rates. Starting in 2026, Medicare is paying separate rates for those with or without APM status (Advanced Alternative Payment Models). The average rates listed above are for non-APM.
Leave A Comment