Healthcare is a highly competitive field, and medical practices routinely find themselves vying for employees, patients, and favorable supplier pricing arrangements. To remain at the top of their game, optimizing operations is essential. Service reimbursements using available CPT codes are one of the primary sources of revenue generation for practices, and remote patient monitoring (RPM) supports this income stream admirably.
The High Costs of Healthcare
U.S. national health is a big-money business. According to the most recent Centers for Medicare & Medicaid Services fact sheet, expenditures grew by 2.7% to $4.3 trillion in 2021, or $12,914 per person. This accounts for a whopping 18.3% of the nation’s Gross Domestic Product (GDP), affecting private and public health payers and individual patients. Healthcare costs are expected to rise from 17.7% of the economy in 2018 to 19.7% by 2028.
Additionally, 60% of Americans have at least one chronic condition, while 40% have two or more. This makes chronic diseases a leading cause of illness, disability, and death, but they are also among the main conditions benefiting from remote patient monitoring services.
How RPM Reimbursements Work
RPM reimbursements are one of the most profitable care management options available. Since the CPT codes were revised in 2020, remote monitoring is now covered by Medicare, Medicaid programs across 34 states, and multiple private payers. Providers receive payment for RPM patient setup and training, followed by a fixed monthly amount for managing health monitoring devices and recording patient readings. In addition, RPM reimbursements cover time spent each month by clinical staff to provide patient care management.
Example CPT Codes for Remote Patient Monitoring Reimbursement
Remote Physiological monitoring (RPM) may be appropriate for patients with at least one acute or chronic disease. Common types of biometric monitoring included weight, blood pressure, blood oxygen saturation, respiratory flow rate, and blood glucose.
Various CPT codes are used for the reimbursement of home health monitors and related services. For example:
- CPT code 99453 yields $19 per patient per month for setting up the initial device and educating the patient on how to use the equipment.
- CPT Code 99454 applies to devices that automatically transmit daily readings and programmed alerts. Provided patients use the devices at least 16 days per month, Medicare pays $56 every 30 days for the supply of the device.
- Under CPT code 99457, Medicare pays $50 per patient per month for clinical staff to spend 20 minutes each month tracking and monitoring data and managing the patient’s care.
- CPT code 99458 provides $41 per month for each additional 20-minute period spent on care management beyond 99457’s initial 20 minutes, up to 60 minutes total.
The amounts listed for remote patient monitoring are approximate based on Medicare’s National Average, and actual reimbursement varies between Medicare administrative contractors (MACs).
Increase Revenue by Adopting an RPM Solution
RPM gives practices of every size and specialty the opportunity to drive recurring revenue. Implementing remote patient monitoring could generate $1,764 per patient each year, as shown in Table 1.
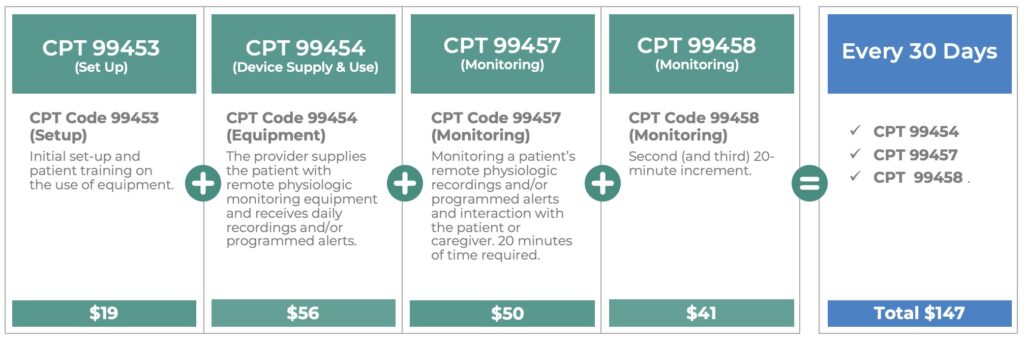
Table 1: How Remote Patient Monitoring reimbursements drive increased practice revenue.
Moreover, by deploying home health monitors that come with system oversight by trained nurses, a practice can triage alerts, reach out to patients to identify the reasons for anomalies, and provide first-level support for technical issues. This delivers several additional benefits beyond the profitability factor.
Additional Benefits of Implementing Remote Patient Monitoring
Oversight of remote health monitoring devices and patient records minimizes the time providers need to spend reviewing the data and managing adherence and other issues. The service reduces strain on in-house medical teams, allowing practices to adopt RPM without needing to employ additional staff to do so. Fewer in-person visits result in less use of resources and increased profitability. These factors reduce the cost of care, improve operational efficiencies, and boost patient satisfaction and retention—all of which contribute to increased profitability.
Discover how to boost your practice revenue and maximize profitability by implementing remote patient monitoring for your patients. For more information, please contact us. Additionally, you can schedule a demo of our RPM program!

Leave A Comment